UHIN has played a pivotal role in a recent Centers for Disease Control and Prevention (CDC) project aiming to track the burden, distribution, and impact of Post-COVID conditions (PCC) in Utah. This initiative, detailed in a study published in BMC Public Health, leverages electronic health records (EHRs) and data from The CHIE (Clinical Health Information Exchange) to identify and analyze cases of PCC, commonly known as long COVID. Researchers aim to understand the prevalence, demographic distribution, and healthcare utilization patterns associated with PCC.
The study provides insights into the long-term effects of COVID-19 and highlights the importance of continuous surveillance to address the ongoing health challenges posed by the pandemic.
UHIN’s Involvement in the Project
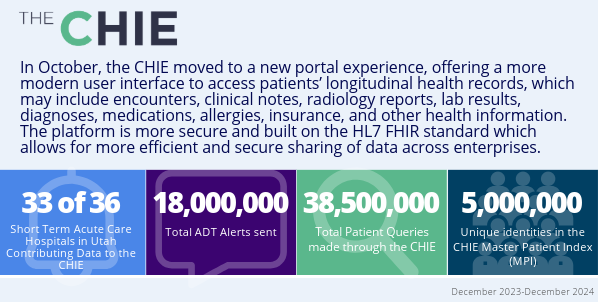
UHIN, as the only HIE in Utah, was an important contributor to this research. Since 1993, we have been committed to reducing healthcare costs and improving the quality of care through secure electronic data interchange. Our extensive network connects healthcare insurers, physicians, hospitals, laboratories, local health departments, and state agencies, enabling seamless data sharing across the state’s healthcare ecosystem.
In this project, UHIN provided a limited dataset including PCC cases and patient trajectories over time. By providing a limited dataset, UHIN was able to support the project, as allowed under HIPAA, while maintaining patient privacy and data integrity.
Collaborative Approach
A collaborative approach fostered partnerships among various healthcare entities, facilitating the aggregation of diverse data sets. Partners in this work are BeyondHIE, Indiana University, Boise State University, the Bronx Regional Health Information Organization (Bronx RHIO) and Comagine Health (our affiliate partner). This inclusivity enabled a more comprehensive understanding of PCC, as data from different sources provided a holistic view of patient experiences and outcomes. UHIN’s commitment to interoperability and data standardization was key to harmonizing information from multiple providers, ensuring consistency and reliability in the study’s findings.
In Conclusion
The success of this project underscores UHIN’s vital role in national health initiatives. By serving as a central hub for health information exchange, UHIN not only supports clinical care but also empowers research efforts that address pressing health concerns. Our infrastructure and expertise in data management are assets in the ongoing battle against COVID-19 and its long-term effects.
Our involvement in this PCC surveillance project adheres to our mission to enhance healthcare through innovation, collaboration, and inclusiveness. By providing the tools and frameworks necessary for comprehensive data analysis, we are proud to continue to contribute significantly to public health research and the improvement of patient care.