UHIN Quarterly Newsletter – Q1 2019
We’ve gone quarterly! Four times a year, UHIN will bring you helpful tips, the latest from Standards, the newest offerings from UHIN, and much more! If you have a comment or if there is a topic you would like to see us cover in an upcoming issue, please email us at communications@uhin.org.
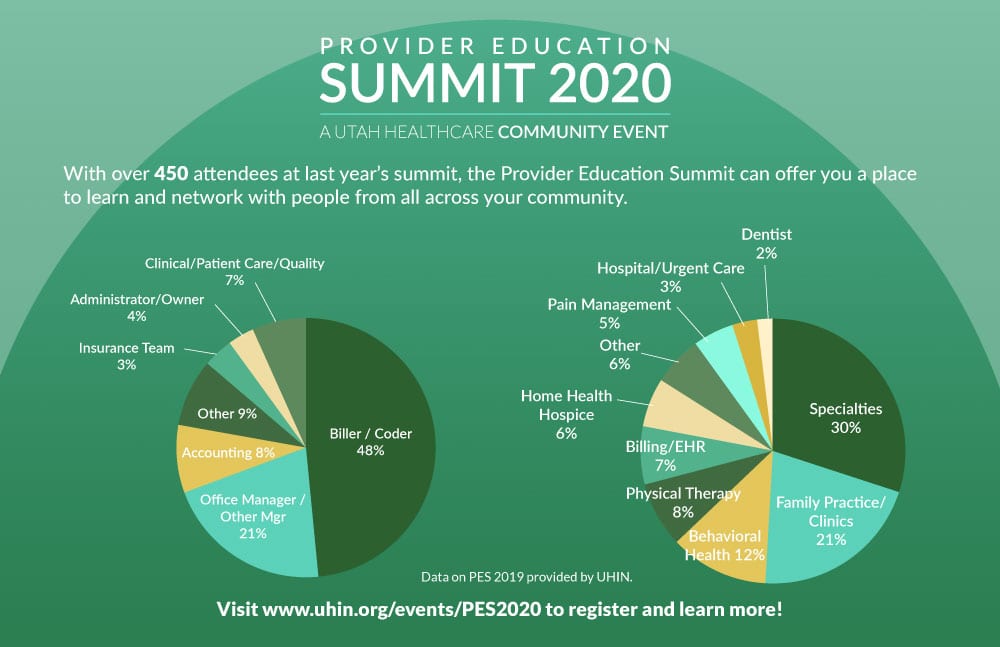
It’s Time for the Provider Education Summits (PES)
Registration is now open for the ever-popular Provider Education Summits (PES)! This free event is just around the corner. A collaboration between multiple healthcare organizations, it features a wide-range of engaging breakout sessions, the always-helpful Payer Panel, interesting vendors, and great prizes.
Last year’s summits attracted more than 400 billers, coders, office managers and other professionals. Register today!
To register, please click on the city that’s best for you.
· Salt Lake – March 19
· Layton – March 20
· Provo – March 27
· St. George – April 3
Attendees who pre-register will be entered into a prize drawing.

The Training Tip
If something goes wrong with the claims billing/reimbursement process, you may need to reach out to someone for help. But whom do you contact? Well, the correct contact will depend on the problem; so, the best strategy is to identify where the process or timeline the problem occurred. You can usually verify this by looking for reports.
Electronic claims trigger a report at each stage, allowing you to track your claim’s progress. Depending on your connections and setup, you may get a confirmation from your claim creation software, an upload/send confirmation, a report from one or more clearinghouses (999/277CA), and up to three reports from the payer (999, 277CA, 835). Most of these confirmations should be available within 24-48 hours of submitting the claim.
Here are some examples of problems that could occur at different stages:
1. You never received a clearinghouse acknowledgement (999 or 277CA) for your claim. Since the clearinghouse never confirmed receipt of the claim, the problem is likely in the claim creation software or in the process of uploading/sending the claims to the clearinghouse. In this case, you should contact your clearinghouse and/or claim creation software vendor for assistance.
2. The claim was acknowledged by the clearinghouse on a 999 or 277CA, but you never got a payer 999 or 277CA. Since the clearinghouse confirmed receipt but the payer did not, the problem most likely occurred when the clearinghouse attempted to send the file to the payer. The best contact in this case is the clearinghouse.
3. The claim was acknowledged by the payer on a 999 and/or 277CA, but the claim has not been paid. Since the payer has confirmed receipt, the claim may be stuck in processing, it may have been pulled for manual review, or they may be waiting for supporting documentation. To find out more, contact the payer’s EDI department. The EDI department is a better choice than customer service since many payer customer service departments cannot see a claim until it has fully adjudicated (i.e. finalized and paid), whereas EDI departments can usually see claims as soon as they are received. If your claim has not adjudicated, make sure to ask for the EDI department.
4. The claim was paid, but you don’t have a remittance (EOB or 835) explaining the payment details. If you normally get paper Explanation of Benefit (EOB) documents in the mail, contact the payer’s customer service department to ensure the EOB was sent to the correct address. If you normally receive electronic 835s, those are passed from the payer back to your clearinghouse; in this case, contact either the payer or the clearinghouse to see if the 835 was generated or delivered, respectively.
Remember, the next time you come across a problem during billing, the first step is to identify where in the process the problem occurred. Did you get any reports? Was the claim rejected at any stage in the process? Which organization was the last one to acknowledge receipt? The answer will guide you to the organization best suited to help you find a solution.

Security Tip
Audits serve an important role in any healthcare organization’s security efforts. Formal audits, conducted by trusted third-party industry organizations, can provide important security accreditation like UHIN’s EHNAC and pending SOC and HITRUST accreditations. However, a self-audit can be the first step in ensuring your office is doing all it can to remain secure while helping to foster a culture of security.
Here are some tips to help you conduct a self-audit before a security issue arises.
Start with your employee handbook. These are the rules and regulations you’ve set in place to ensure that your company runs smoothly and securely. You want to verify that your staff is following the rules you’ve created.
Focus on the security section of your handbook. It’s a great idea to do audits on other sections as well, but for security it isn’t as important if your office has a set number of holidays.
After reviewing the rules you’ve created, have your IT department run a few simple reports that will help you verify that your regulations are being followed. Some of the areas you want to check to ensure the best security practices are being followed are:
· Passwords are being changed on a regular basis (UHIN and other industry experts recommend passwords be updated every 90 days)
· Access to emails and other tools with sensitive data was eliminated immediately after former employees left
· Websites are limited to those needed for employees to successfully do their jobs (thus reducing the chances of viruses)
· Medical records are accessed only by those who have a HIPAA-approved need to see them (UHIN can help you with a CHIE-access audit)
Next, do a physical audit. Some items to be conscious of:
· Computers that are still logged into when not in use
· Drawers and cabinets containing important information you find unlocked
· Doors leading to areas with sensitive information not properly secured
· Post-it notes with login and password information
All of these are a security hazard!
Once you’ve completed your internal security audit, use it as an opportunity to educate your staff about best practices. Barring a HIPAA violation, which would likely require a deeper investigation, and depending on your employee handbook, there’s probably no need for disciplinary action following the audit.
Remember, a self-audit is a great first step to improving security and helping to foster a culture centered around security!
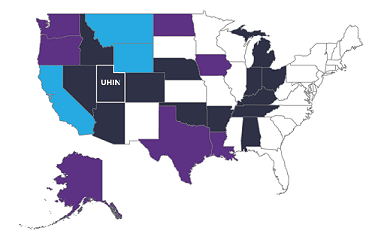
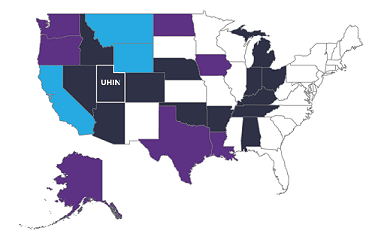
Patient-Centered Data Home (PCDH) Keeps on Growing
The Strategic Health Information Exchange Collaborative’s (SHIEC) efforts to expand interoperability through nationwide connectivity continues to advance. Alabama’s HIE, One Health Record, is now sharing vital patient data with SHIEC’s PCDH Western Implementation, of which UHIN is a founding member.
With the inclusion of One Health Record, providers in any of the participating PCDH HIEs can now safely and securely coordinate care for over 2.5 million patients who may seek care in one of the other participating HIE’s jurisdictions. And Utahns who experience a medical encounter in one of 23 hospitals and over 70 other Alabama facilities can rest assured their Utah doctor will be notified via CHIE Alert.
The Cotton State is one of 22 states participating in the PCDH. More are in the process of joining every day.

New from UHIN
UHIN continually adds new features and offerings. We’re pleased to announce our latest additions:
- UTRANSEND members can now conveniently upload attachments using a modern web implementation. The new feature allows payers and providers to communicate with one another to advance the claim attachment process and help expediate payments. Users can search, filter, print, accept, reject and even archive their claim attachments. Additionally, a graphical tracker helps users to visualize the current status of the claim attachment – keeping them in the loop every step of the way! Currently, Medicaid is the only payer actively accepting attachments, but more payers are expected to follow suit soon.
- UHIN’s CHIE Alerts, notifying subscribers of ADT information have become even more helpful. Past encounter information for inpatient and emergency encounters over the last 90 days is now available. This information is invaluable to reducing hospital readmissions and improving patient care. If you’d like to have Past Encounter Information included in your ADT Alerts, please contact customerservice@uhin.org.

Standards: What’s New in the Standards Committee?
There’s a new home for Standards Committee information on the UHIN website! The Standards Committee is open to the public; therefore, everyone is welcome to visit UHIN’s Knowledgebase section for Standards Committee Information to see minutes from the meetings, graphs of the standards process, and even the charter for the Standards Committee. If you have questions or would like to get involved, contact standards@uhin.org.
On the national stage, important conversations have been brewing about how to improve the standards-development process. There have been concerns in the industry that the process to create and update standards is too cumbersome and slow to keep pace with the nation’s needs. To address this, NCVHS, an advisory body to Health & Human Services (HHS), has published a letter to the Secretary of HHS with a number of bold recommendations designed to provide solutions.
Other new developments include a new Utah standard to address the Applied Behavioral Analysis (ABA) code updates and their usage, a recent webinar by Dr. Mirella Petersen explaining the code updates and providing examples, and discussions on the national level about adding the ability to send a 277CA report with an acceptance and a warning. Stay tuned for future updates!

In the News
UHIN’s president and CEO, Teresa Rivera, was recently featured in Healthcare Finance in advance of her HIMSS 2019 presentation. You can read the news article here. Click here to download the slides from Teresa’s HIMSS 2019 presentation.

UHIN’s New Website
UHIN has launched a new, more user-friendly website! Check it out at www.uhin.org.
What’s on Your Correspondent’s Mind? Whose Records Are They Anyway?
Recently, your intrepid correspondent had his first exam with a new primary care physician. The flow of his records from his former physician to his new one was infinitely easier than when he changed doctors after moving from L.A. to Salt Lake. A call to his former California doctor’s office found him in an argument with the front desk person who told him she would only send the records to a new provider. This caused your mild-mannered correspondent to shout, “Whose records are they anyway?” Thanks to movements like OpenNotes, providers and payers alike are beginning to understand that those medical records belong to the patient. With UHIN’s beta patient portal, MYONECHART, patients can view all their aggregated records found in the CHIE – eliminating the need to log into multiple portals. If you want to share anything with your correspondent, he can be reached at communications@uhin.org.